The changes of brain electric activity in patients with different severity of coronary atherosclerosis one-year after coronary artery bypass grafting
https://doi.org/10.17802/2306-1278-2020-9-1-6-14
Abstract
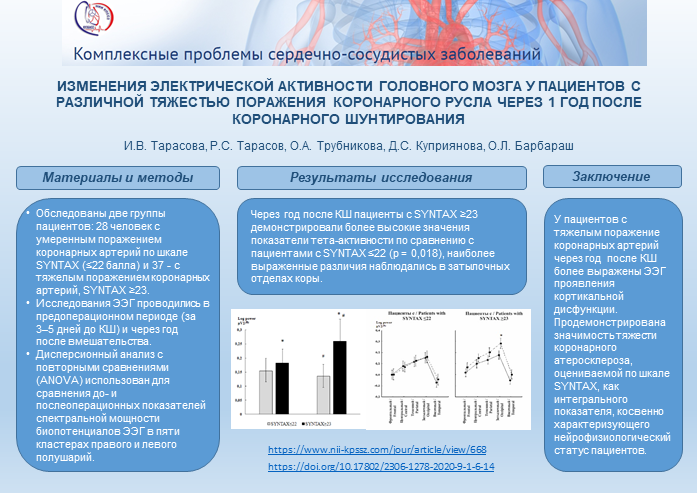
Aim.To examine the brain electrical activity changes with the quantitative electroencephalogram (qEEG) indicators (the spectral power) in patients at 1 year after on-pump coronary artery bypass grafting (CABG) depending on the severity of the coronary lesions.
Methods.65 patients were included in the study. Before performing CABG, they were divided into two groups depending on the severity of coronary artery disease according to the SYNTAX score: patients with mild coronary artery lesions – SYNTAX ≤22, (n = 28) and patients with severe coronary lesions – SYNTAX ≥ 23, (n = 37). EEG studies were performed in the preoperative period (at days 3–5 before GABG) and 1 year after surgery. Variance analysis with repeated comparisons (ANOVA) was used to compare pre-and postoperative EEG spectral power indicators in five clusters of the right and left hemispheres.
Results.Patients with SYNTAX ≥23 had higher theta rhythm power values as compared with patients with SYNTAX ≤22 (p = 0.018) at 1 year after CABG, whereas these groups were comparable before the surgery. In addition, patients with severe lesions of the coronary arteries (SYNTAX ≥23) demonstrated an increase of theta rhythm power at 1 year after surgery in comparison to preoperative values (p = 0.017), this effect was not detected in patients with SYNTAX ≤22.
Conclusion.One year after CABG, patients with severe coronary lesions (SYNTAX ≥23), demonstrated qEEG changes that resembled cortical dysfunction, showing significance of severity of coronary atherosclerosis, assessed by the SYNTAX score, as an integral indicator, indirectly characterizing neurophysiological status of patients.About the Authors
I. V. TarasovaRussian Federation
Tarasova Irina V.- PhD, leading researcher at the Laboratory of Ultrasound and Electrophysiological Research Methods, Department of Cardiovascular Disease Diagnosis, Federal State Budgetary Institution "Research Institute for Complex Issues of Cardiovascular Diseases".
6, Sosonoviy Blvd., Kemerovo, Russian Federation, 650002
R. S. Tarasov
Russian Federation
Tarasov Roman S.-PhD, Head of the Laboratory for Reconstructive Surgery of Multivessel and Polyvascular Disease, Federal State Budgetary Institution "Research Institute for Complex Issues of Cardiovascular Diseases".
6, Sosonoviy Blvd., Kemerovo, Russian Federation, 650002
O. A. Trubnikova
Russian Federation
Trubnikova Olga A.-PhD, Head of the Laboratory of Neurovascular Pathology, Department of Multivessel and Polyvascular Disease, Federal State Budgetary Institution "Research Institute for Complex Issues of Cardiovascular Diseases".
6, Sosonoviy Blvd., Kemerovo, Russian Federation, 650002
D. S. Kupriyanova
Russian Federation
Kupriyanova Darya S.-laboratory assistant at the Laboratory of Ultrasound and Electrophysiological Research Methods, Department of Cardiovascular Disease Diagnosis, Federal State Budgetary Institution "Research Institute for Complex Issues of Cardiovascular Diseases".
6, Sosonoviy Blvd., Kemerovo, Russian Federation, 650002
O. L. Barbarash
Russian Federation
Barbarash Olga L.- PhD., Professor, Corresponding Member of the RAS, Director of the Federal State Budgetary Institution "Research Institute for Complex Issues of Cardiovascular Diseases".
6, Sosonoviy Blvd., Kemerovo, Russian Federation, 650002
References
1. Aono J., Ikeda S., Katsumata Y., Higashi H., Ohshima K., Ishibashi K., Matsuoka H., Watanabe K., Hamada M. Correlation between plaque vulnerability of aorta and coronary artery: an evaluation of plaque activity by direct visualization with angioscopy. Int J Cardiovasc Imaging. 2015; 31(6): 11071114. doi: 10.1007/s10554-015-0669-z.
2. Tao H., Wang Y., Zhou X., Zhong W., Zhou H., Li K., Zhao B. Angiographic correlation and synergistic effect of coronary artery stenosis and cerebral artery stenosis: a retrospec-tive study. Med Sci Monit. 2014; 20:1902-1907. doi: 10.12659/MSM.892271.
3. Emmert M.Y., Grünenfelder J., Scherman J., Cocchieri R., van Boven W.J., Falk V., Salzberg S.P. HEARTSTRING enabled no-touch proximal anastomosis for off-pump coronary artery bypass grafting: current evidence and technique. Interact Cardiovasc Thorac Surg. 2013; 17(3): 538-41. doi: 10.1093/icvts/ivt237.
4. Pawliszak W, Kowalewski M, Raffa GM, Malvindi PG, Kowalkowska ME, Szwed KA, Borkowska A, Kowalewski J, Anisimowicz L. Cerebrovascular events after no-touch offpump coronary artery bypass grafting, conventional side-clamp off-pump coronary artery bypass, and proximal anastomotic devices: a meta-analysis. J Am Heart Assoc. 2016; 5(2). pii: e002802. doi: 10.1161/JAHA.115.002802.
5. Yadav M. Palmerini T., Caixeta A., Madhavan M.V., Sanidas E., Kirtane A.J., Stone G.W., Genereux P. Prediction of coronary risk by SYNTAX and derived scores: synergy between percutaneous coronary intervention with taxus and cardiac surgery. J Am Coll Cardiol. 2013;62(14):1219-1230. doi: 10.1016/j.jacc.2013.06.047
6. Tarasova I.V., Tarasov R.S., Trubnikova O.A., Barbarash O.L., Barbarash L.S. SYNTAX score effect on electroencephalography power dynamics in patients undergoing on-pump coronary artery bypass grafting. BMC Neurosci. 2013; 14: 95. doi: 10.1186/1471-2202-14-95.
7. Tarasova I.V., Kukhareva I.N., Barbarash O.L. EEG markers of cognitive impairments in patients with coronary artery disease. Nevrologiya, neiropsikhiatriya, psikhosomatika. 2016; 8(3): 43– 47. doi: 10.14412/2074-2711-2016-3-43-47 (In Russian)
8. Başar E. Brain oscillations in neuropsychiatric disease. Dialogues Clin Neurosci. 2013; 15(3): 291-300. 9. Sutter R., Kaplan P.W., Cervenka M.C., Thakur K.T., Asemota A.O., Venkatesan A., Geocadin R.G. Electroencephalography for diagnosis and prognosis of acute encephalitis. Clin Neurophysiol. 2015; 126(8): 1524-1531. doi: 10.1016/j.clinph.2014.
9. Tarasova I.V., Maleva O.V., Chernobay A.G., Barbarash O.L., Barbarash L.S. The effect of mild cognitive impairment on the brain bioelectrical activity changes in patients undergoing coronary artery bypass surgery with cardiopulmonary bypass. Neurological Journal. 2015; 20(5): 20-25. (In Russian)
10. Wabulya A., Lesser R.P., Llinas R., Kaplan P.W. Electroencephalography and brain MRI patterns in encephalopathy. Clin EEG Neurosci. 2016; 47(2): 150-156. doi: 10.1177/1550059415590058.
11. Reineke D., Winkler B., König T., Meszaros K., Sodeck G., Schönhoff F., Erdoes G., Czerny M., Carrel T. Minimized extracorporeal circulation does not impair cognitive brain function after coronary artery bypass grafting. Interact Cardiovasc Thorac Surg. 2015; 20(1):68-73. doi: 10.1093/icvts/ivu341.
12. Tarasova I.V., Maleva O.V., Tarasov R.S., Barbarash O.L., Barbarash L.S. The effect of mild cognitive impairment on EEG topographic changes after on-pump coronary artery bypass grafting. Kompleksnye problemy serdechno-sosudistyh zabolevanij. 2017; 1: 37-43. (In Russian)
13. Trubnikova O.A., Tarasova I.V., Maleva O.V., Kagan E.S., Barbarash O.L., Barbarash L.S. Factors for the development of persistent postoperative cognitive dysfunction in patients undergoing coronary artery bypass surgery under extracorporeal circulation. Terapevticheskiy arkhiv. 2017; 89(9): doi: 41-47. 10.17116/terarkh201789941-47 (In Russian)
14. Volf N.V., Tarasova I.V., Razumnikova O.M. Genderrelated differences in changes in the coherence of cortical biopotentials during image-based creative thought: relationship with action efficacy. Neurosci Behav Physiol. 2010; 40(7): 793799. doi: 10.1007/s11055-010-9328-y.
15. Golukhova E.Z., Polunina A.G., Lefterova N.P., Morelli O.D., Begachyov A.V. Electroencephalography as a tool for the diagnosis of ischemic changes in the brain after coronary artery bypass grafting. Creative cardiology. 2012; 1: 107-122. (In Russian)
16. Tarasova I.V., Vol'f N.V., Syrova I.D., Barbarash O.L., Barbarash L.S. Mild cognitive impairment in patients with coronary artery disease: clinical-demographyc and EEGcorrelates. Zh Nevrol Psikhiatr Im S S Korsakova. 2014; 114(12): 89-93. doi: 10.17116/jnevro201411412189-93. (In Russian)
17. Goto T., Maekawa K. Cerebral dysfunction after coronary artery bypass surgery. J Anesth. 2014; 28(2): 242-248. doi: 10.1007/s00540-013-1699-0.
18. Halkos M.E., Anderson A., Binongo J.N.G., Stringer A., Lasanajak Y., Thourani V.H., Lattouf O.M., Guyton R.A., Baio K.T., Sarin E., Keeling W.B., Cook N.R., Carssow K., Neill A., Glas K.E., Puskas J.D. Operative strategies to reduce cerebral embolic events during on- and off-pump coronary artery bypass surgery: A stratified, prospective ran-domized trial. J Thorac Cardiovasc Surg. 2017 Jun 16. pii: S0022-5223(17)31226-6. doi: 10.1016/j.jtcvs.2017.04.089.
19. Martínez-Comendador J., Alvarez J.R., Sierra J., Teijeira E., Adrio B. Preoperative statin therapy in cardiac surgery is more effective in patients who display preoperative activa-tion of the inflammatory system. Tex Heart Inst J. 2013; 40(1): 42-49.
20. Miyazaki S., Yoshitani K., Miura N., Irie T., Inatomi Y., Ohnishi Y., Kobayashi J. Risk factors of stroke and delirium after off-pump coronary artery bypass surgery. Interact Cardiovasc Thorac Surg. 2011; 12(3): 379-383. doi: 10.1510/ icvts.2010.248872.
21. Kovacevic P., Redzek A., Kovacevic-Ivanovic S., Velicki L., Ivanovic V., Kieffer E. Coronary and carotid artery occlusive disease: single center experience. Eur Rev Med Pharmacol Sci 2012; 16(4): 483-490.
22. Tang T.Y., Howarth S.P., Miller S.R., Graves M.J., U-KingIm J.M., Li Z.Y., Walsh S.R., Hayes P.D., Varty K., Gillard J.H. Comparison of the inflammatory burden of truly asymptomatic carotid atheroma with atherosclerotic plaques in patients with asymptomat-ic carotid stenosis undergoing coronary artery bypass grafting: an ultrasmall superpara-magnetic iron oxide enhanced magnetic resonance study. Eur J Vasc Endovasc Surg. 2008; 35(4): 392-398. doi: 10.1016/j.ejvs.2007.10.019.
23. Masabni K., Sabik J.F., Raza S., Carnes T., Koduri H., Idrees J.J., Beach J., Riaz H., Shishehbor M.H., Gornik H.L., Blackstone E.H. Nonselective carotid artery ultrasound screening in patients undergoing coronary artery bypass grafting: Is it necessary? J Thorac Cardiovasc Surg. 2016; 151(2): 402-408. doi: 10.1016/j.jtcvs.2015.09.108.
Review
For citations:
Tarasova I.V., Tarasov R.S., Trubnikova O.A., Kupriyanova D.S., Barbarash O.L. The changes of brain electric activity in patients with different severity of coronary atherosclerosis one-year after coronary artery bypass grafting. Complex Issues of Cardiovascular Diseases. 2020;9(1):6-14. (In Russ.) https://doi.org/10.17802/2306-1278-2020-9-1-6-14








































