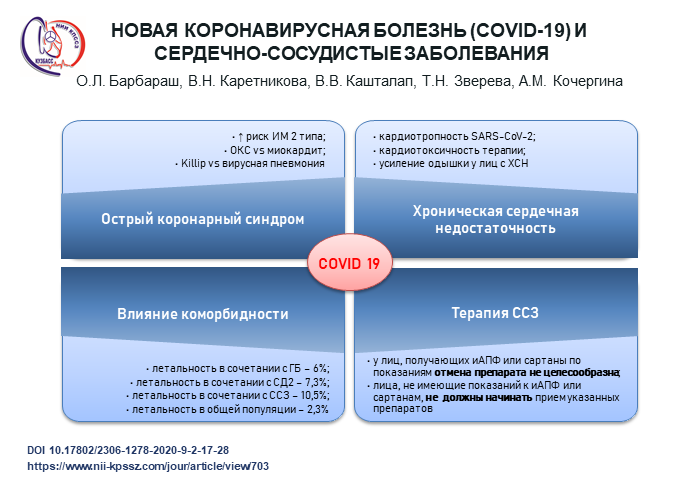
New coronavirus disease (COVID-19) and cardiovascular disease
https://doi.org/10.17802/2306-1278-2020-9-2-17-28
Abstract
The management of these patients requires healthcare professionals to have specific knowledge on the characteristics of the viral infection, its clinical signs and symptoms combined with cardiovascular diseases, as well as individual and collective prevention measures. The safety of healthcare professionals and favorable prognosis of patients are of the top priority for the modern healthcare system.
The review discusses current challenges associated with the novel coronavirus disease COVID-19 and cardiovascular diseases. The results of few clinical trials and individual case reports have shown the presence of certain problems in treating patients with comorbidity and viral infection. The new data on the drug interactions are reported. Common patterns of typical cardiovascular diseases and COVID-19 are presented. The risk groups with the need for timely diagnosis and intensive cardiac care are identified to prevent adverse outcomes in patients with this comorbidity.
About the Authors
O. L. BarbarashRussian Federation
Barbarash Olga L. - MD, PhD, Professor, Corresponding Member of the RAS, Director RICICD; Head of the Department of Cardiology and Cardiovascular Surgery, KemSMU.
6, Sosonoviy Blvd., Kemerovo, 650002; 22a, Voroshilova St., Kemerovo, 650029
Competing Interests: not
V. N. Karetnikova
Russian Federation
Karetnikova Victoria N. - MD, PhD, Professor, Head of the Laboratory of Circulatory Pathology at the Department of Clinical Cardiology, RICICD; Professor at the Department of Cardiology and Cardiovascular Surgery, KemSMU.
6, Sosonoviy Blvd., Kemerovo, 650002; 22a, Voroshilova St., Kemerovo, 650029
Competing Interests: not
V. V. Kashtalap
Russian Federation
Kashtalap Vasily V. - MD, PhD, Associate Professor, Head of the Department of Clinical Cardiology at the RICICD; Associate Professor at the Department of Cardiology and Cardiovascular Surgery, KemSMU.
6, Sosonoviy Blvd., Kemerovo, 650002; 22a, Voroshilova St., Kemerovo, 650029
Competing Interests: not
T. N. Zvereva
Russian Federation
Zvereva Tatiana N. - MD, PhD, research associate at the Rehabilitation Laboratory, Department of Clinical Cardiology, RICICD; Associate Professor at the Department of Cardiology and Cardiovascular Surgery, KemSMU.
6, Sosonoviy Blvd., Kemerovo, 650002; 22a, Voroshilova St., Kemerovo, 650029
Competing Interests: not
A. M. Kochergina
Russian Federation
Kochergina Anastasia M. - MD, PhD, researcher at the Laboratory of Circulatory Pathology, Department of Clinical Cardiology, RICICD; assistant lecturer at the Department of Cardiology and Cardiovascular Surgery, KemSMU.
6, Sosonoviy Blvd., Kemerovo, 650002; 22a, Voroshilova St., Kemerovo, 650029
Competing Interests: not
References
1. Guan W.J., Ni Z.Y., Hu Y, Liang W., Ou Ch., He J. et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020; 2020 Feb 28. doi: 10.1056/NEJMoa2002032.
2. Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19). 16-24 February 2020. Available at: https://wwwwhoint/docs/default-source/coronaviruse/who-china-joint-mission-on-covid-19-final-reportpdf (accessed March 9, 2020.
3. Shlyakhto E. V, Konradi A. O., Arutyunov G. P., Arutyunov A. G., Bau- tin A. E., Boytsov S. A., Villevalde S. V., Grigoryeva N. Yu.,Duplyakov D. V, Zvar- tau N. E., Koziolova N. A., Lebedev D. S., Malchikova S. V, Medvedeva E. A., Mikhailov E. N., Moiseeva O. M., Orlova Ya. A., Pavlova T. V, Pevsner D. V, Petrova M. M., Rebrov A. P., Sitnikova M. Yu.,Solovyova A. E., Tarlovskaya E. I., Truk- shina M. A., Fedotov P. A., Fomin I. V, Khripun A. V, Chesnikova A. I., Shaposhnik I. I., Yavelov I. S., Yakovlev A. N. Guidelines for the diagnosis and treatment of circulatory diseases in the context of the COVID-19 pandemic. Russian Journal of Cardiology. 2020;25(3):3801. (In Russian) doi:10.15829/1560-4071-2020-3-3801.
4. Driggin E., Madhavan M.V., Bikdeli B., Chuich T., Laracy J., Bondi-Zoccai G. et al Cardiovascular Considerations for Patients, Health Care Workers, and Health Systems During the Coronavirus Disease 2019 (COVID-19) Pandemic. J Am Coll Cardiol. 2020 Mar 19. Epublished Doi:10.1016/j.jacc.2020.03.031.
5. Li B., Yang J., Zhao F., Zhi L., Wang X., Liu L., Bi Z., Zhao Yu. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020 Mar 11; 1-8 doi: 10.1007/s00392-020-01626-9
6. Wu Z., Mc Googan J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020. Feb 24. doi: 10.1001/jama.2020.2648.
7. Porcheddu R., Serra C., Kelvin D., Kelvin N., Rubino S. Similarity in Case Fatality Rates (CFR) of COVID-19/SARS-COV-2 in Italy and China. J Infect Dev Ctries. 2020;14:125-128. doi: 10.3855/jidc.12600.
8. Chen N., Zhou M., Dong X., Qu J., Gong F., Ya. Han et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507-513. doi: 10.1016/S0140-6736(20)30211-7.
9. Liu W.M., Vander Zeijst B.A., Boog C.J., Soethout E.C. Aging and impaired immunity to influenza viruses: implications for vaccine development. HumVaccin. 2011; 7 Suppl: 94-8.
10. Zidar D.A., Al-Kindi S.G., Liu Y, Krieger N.I., Perzynski A.T., Osnard M. et al. Association of Lymphopenia With Risk of Mortality Among Adults in the US General Population. JAMA. Netw Open 2019;2:e1916526 doi: 10.1001/jamanetworkopen.2019.16526.
11. Saltiel A.R., Olefsky J.M. Inflammatory mechanisms linking obesity and metabolic disease. J Clin Invest. 2017;127:1-4
12. Akhmerov A., Marban E. COVID-19 and the Heart. Circulation. 2020Apr 11. doi: 10.1161/CIRCRESAHA. 120.317055.
13. Inciardi R.M., Lupi L., Zaccone G., Italia L., Raffo M., Tomasonit D. et al. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020; DOI: 10.1001/jamacardio.2020.1096.
14. ZhengY-Y., MaY.-T., Zhang J.-Y., Xie X. COVID-19 and the cardiovascular system. Nature Reviews Cardiology. 2020. Mar 5. doi: 10.1038/s41569-020-0360-5.
15. Ganatra S., Hammond S.P., Nohria A. The Novel Coronavirus Disease (COVID-19) Threat for Patients with Cardiovascular Disease and Cancer JACC: Cardio Oncology. 2020. doi: 10.1016/j.jaccao.2020.03.001.
16. Mortality G.B.D., Causes of Death C. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1459-1544.
17. Liang W., Guan W., Chen Retal. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335-337.
18. Guo T., FanY, Chen M., Wu X., Zhang L., He T., Wang H., Wan J., Wang X., Lu Z. Cardiovascular Implications of Fatal Outcomes of Patients With Coronavirus Disease 2019 (COVID-19). JAMACardiol. 2020 Mar 27. doi: 10.1001/jamacardio.2020.1017.
19. Sharon E. Fox, Aibek Akmatbekov, Jack L. Harbert, Guang Li, J. Quincy Brown, Richard S. Vander Heide. Pulmonary and Cardiac Pathology in Covid-19: The First Autopsy Series from New Orleans. medRxiv. https://www.medrxiv.org/content/10.1101/2020.04.06.20050575v1/ doi:https://doi.org/10.1101/2020.04.06.20050575.
20. Welt F.G.P., Shah P.B., Aronow H.D., Bortnick A.E., Henry T.D., Sherwood M.W., Young M.N., Davidson L.J., Kadavath S., Mahmud E., Kirtane A.J., American College of Cardiology’s (ACC) Interventional Council and the Society of Cardiovascular Angiography and Intervention (SCAI), Catheterization Laboratory Considerations During the Coronavirus (COVID-19) Pandemic: From ACC’s Interventional Council and SCaI. J Am Coll Cardiol. 2020 Mar 16; S0735-1097(20)34566-6. doi: 10.1016/j.jacc.2020.03.021..
21. Bettari L., Pero G., Maiandi C., Messina A., Saccocci M., Cirillo M., Troise G., Conti E., Cuccia C., Maffeo D. Exploring personal protection during high-risk PCI in a COVID-19 patient -Impella CP mechanicalsupportduring ULMCA bifurcationstenting. JACC: CaseReports. April 2020 DOI: 10.1016/j.jaccas.2020.03.006.
22. Fried J.A., Ramasubbu K., Bhatt R., Topkara V.K., Clerkin K.J., Horn E. et al. The Variety of Cardiovascular Presentations of COVID-19. Circulation. 2020 Apr 3. doi: 10.1161/CIRCULATIONAHA.120.047164.
23. Juneman E. Leading the compassionate charge. Circ Heart Fail. 2020 Apr;13(4):e007085. doi: 10.1161/CIRCHEARTFAILURE.120.007085.
24. Oudit G. Y, Kassiri Z., Jiang C., Liu P.P., Poutanen S.M., Penninger J.M., Butany J. SARS-coronavirus Modulation of Myocardial ACE2 Expression and Inflammation in Patients With SARS Eur J Clin Invest. 2009 Jul; 39(7):618-25. doi: 10.1111/j.1365-2362.2009.02153.x.
25. Haeck G., Ancion A., Marechal P, Oury C., Lancellotti P. COVID-19 andcardiovascular diseases. Rev Med Liege. 2020 Apr;75(4):226-232.
26. Huang C., Wang Y, Li X., Ren L., Zhao J., Hu Y, Zhang L., Fan G., Xu J., Gu X. et al Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020 Feb 15;395(10223):497-506. doi: 10.1016/S0140-6736(20)30183-5.
27. Wang D. , Hu B. , Hu C., Zhu F. , Liu X. , Zhang J. , et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020 Feb 7. doi: 10.1001/jama.2020.1585.
28. Dong N., Cai J., Zhou Y, Liu J., Li F., End-stage Heart Failure with COVID-19: Strong Evidence of Myocardial Injury by 2019-nCoV, JACC Heart Fail. 2020 Apr 7. pii: S2213-1779(20)30200-6. doi: 10.1016/j.jchf.2020.04.001.
29. Sakabe M., Yoshioka R., Fujiki A. Sick sinus syndrome induced by interferon and ribavirin therapy in a patient with chronic hepatitis C. J. Cardiol. Cases. 2013 Oct 29;8(6):173-175. doi: 10.1016/j.jccase.2013.08.002.
30. Al Ghamdi M., Mushtaq F., Awn N., Shalhoub S. MERS CoV Infection in Two Renal Transplant Recipients: Case Report. Am J Transplant. 2015;15:1101-1104.
31. Kumar D., Tellier R., Draker R., Levy G., Humar A. Severe Acute Respiratory Syndrome (SARS) in a Liver Transplant Recipient and Guidelines for Donor SARS Screening. Am J Transplant. 2003;3:977-981.
32. Li F., Cai Jand Dong N. First Cases of COVID-19 in Heart Transplantation From China. J Heart Lung Transplant. 2020. doi: 10.1016/j.healun.2020.03.006.
33. Ren Z.-Li, Hu R., Wang Z.-W., Zhang M., Ruan Y-L., Wu Z.-Y et al Epidemiological and Clinical Characteristics of Heart Transplant Recipients During the 2019 Coronavirus Outbreak in Wuhan, China: A Descriptive Survey Report. J Heart Lung Transplant. 2020. doi: 10.1016/j.healun.2020.03.008.
34. Guidance for Cardiothoracic Transplant and Mechanical Circulatory Support Centers regarding SARS CoV-2 infection and COVID-19: March 17, 2020. Available at: https://community.ishlt.org/HigherLogic/System/DownloadDocumentFile. ashx?DocumentFileKey=afb06f06-5d63-1 3d4-c107-d152a9f6cd46. (accessed 13.03.2020)
35. American Society of Transplantation. 2019-nCoV (Coronavirus): FAQs for Organ Transplantation. Updated Feb 29, 2020. Available at: https://www.myast.org/sites/default/files/COVID19%20FAQ%20Tx%20Centers%20030220-1.pdf. (accessed 13.03.2020)
36. Prognostic Factors in COVID-19 Patients Complicated With Hypertension (NCT04272710) Available at: https://clinicaltrials.gov/ct2/show/NCT04292964. accessed (14.03.2020)
37. 3 7. Kuster G.M., Pfister O., Burkard T., Zhou Q., Twerenbold R., Haaf Ph., Widmer A.F., Osswald S. SARS-CoV2: should inhibitors of the renin-angiotensin system be with drawn in patients with COVID-19? European Heart Journal. 2020 doi: 10.1093/eurheartj/ehaa235.
38. University of Liverpool. Interactions with Experimental COVID-19 Therapies. Available at: https://www.Covid19-druginteractions.org (accessed 13.04.2020)
39. Virani S.S. Is There a Role For Statin Therapy in Acute Viral Infections? Available at: https://www.acc.org/latest-in-cardiology/articles/2020/03/18/15/09/is-there-a-role-for-statin-therapy-in-acute-viral-infections-covid-19. (accessed 14.04.2020)
40. Liu W., Li H. COVID-19: Attacks the 1-Beta Chain of Hemoglobin and Captures the Porphyrin to Inhibit Human Heme Metabolism Available at: https://chemrxiv.org (accessed 14.04.2020)
41. Thachil J., Tang N., Gando S., Falanga A., Cattaneo M., Levi M., Clark C., Iba T. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost. 2020 25 March 25. doi:10.1111/JTH.14810.
42. Tang N., Bai H., Chen X., Gong J., Li D., Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. 2020 Mar 27. doi: 10.1111/jth.14817.
43. Hunt B., Retter A., McClintock C. Practical guidance for the prevention of thrombosis and management of coagulopathy and disseminated intravascular coagulation of patients infected with COVID-19. Available at: https://thrombosisuk.org/downloads/T&H%20and%20COVID.pdf (accessed 14.04.2020.)
44. COVID-19 Clinical Guidance For the Cardiovascular Care Team. ACC CLINICAL BULLETIN. https://www.acc.org/latest-in-cardiology/features/~/media/Non-Clinical/Files-PDFs-Excel-MS-Word-etc/2020/02/S20028-ACC-Clinical-Bulletin-Coronavirus.pdf. (accessed 13.04.2020)
Supplementary files
|
|
1. Графическое резюме | |
| Subject | ||
| Type | Исследовательские инструменты | |
View
(76KB)
|
Indexing metadata ▾ | |
Review
For citations:
Barbarash O.L., Karetnikova V.N., Kashtalap V.V., Zvereva T.N., Kochergina A.M. New coronavirus disease (COVID-19) and cardiovascular disease. Complex Issues of Cardiovascular Diseases. 2020;9(2):17-28. (In Russ.) https://doi.org/10.17802/2306-1278-2020-9-2-17-28








































